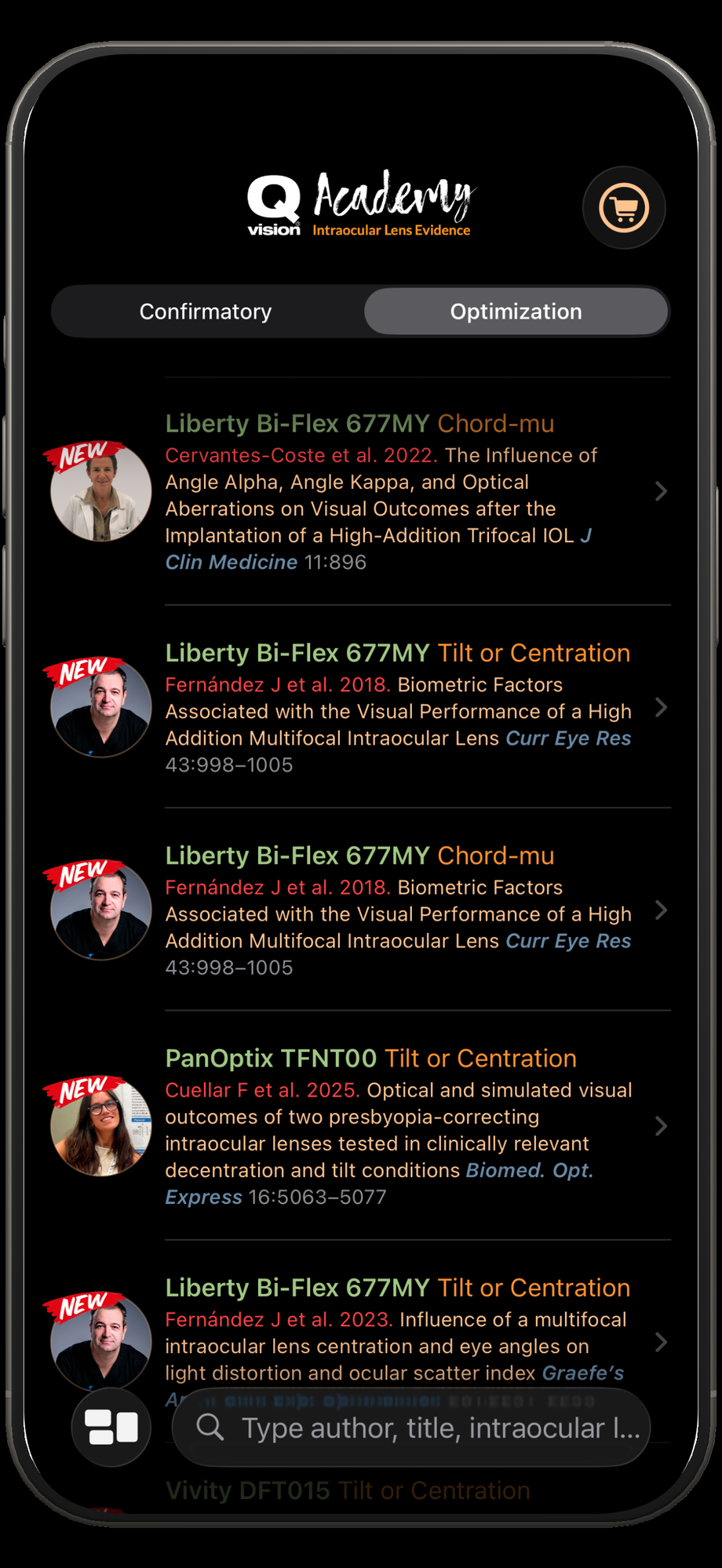
1.4. Read an Optimization Report
Optimization Reports are designed to help clinicians understand why clinical outcomes associated with an intraocular lens (IOL) may vary across patients, studies, or surgical approaches. While Confirmatory Reports focus on standardized outcomes to classify the functional behavior of an IOL, Optimization Reports explore variability, identifying the factors that modify performance in real-world conditions.
These reports are particularly useful for translating evidence into individualized clinical decisions. They allow clinicians to interpret outcomes beyond averages, understand conflicting results across studies, and optimize lens selection and surgical planning for specific patient profiles.
Each Optimization Report follows a fixed, clinician-centered template to ensure consistency, clarity, and practical relevance.
 |  |
|---|
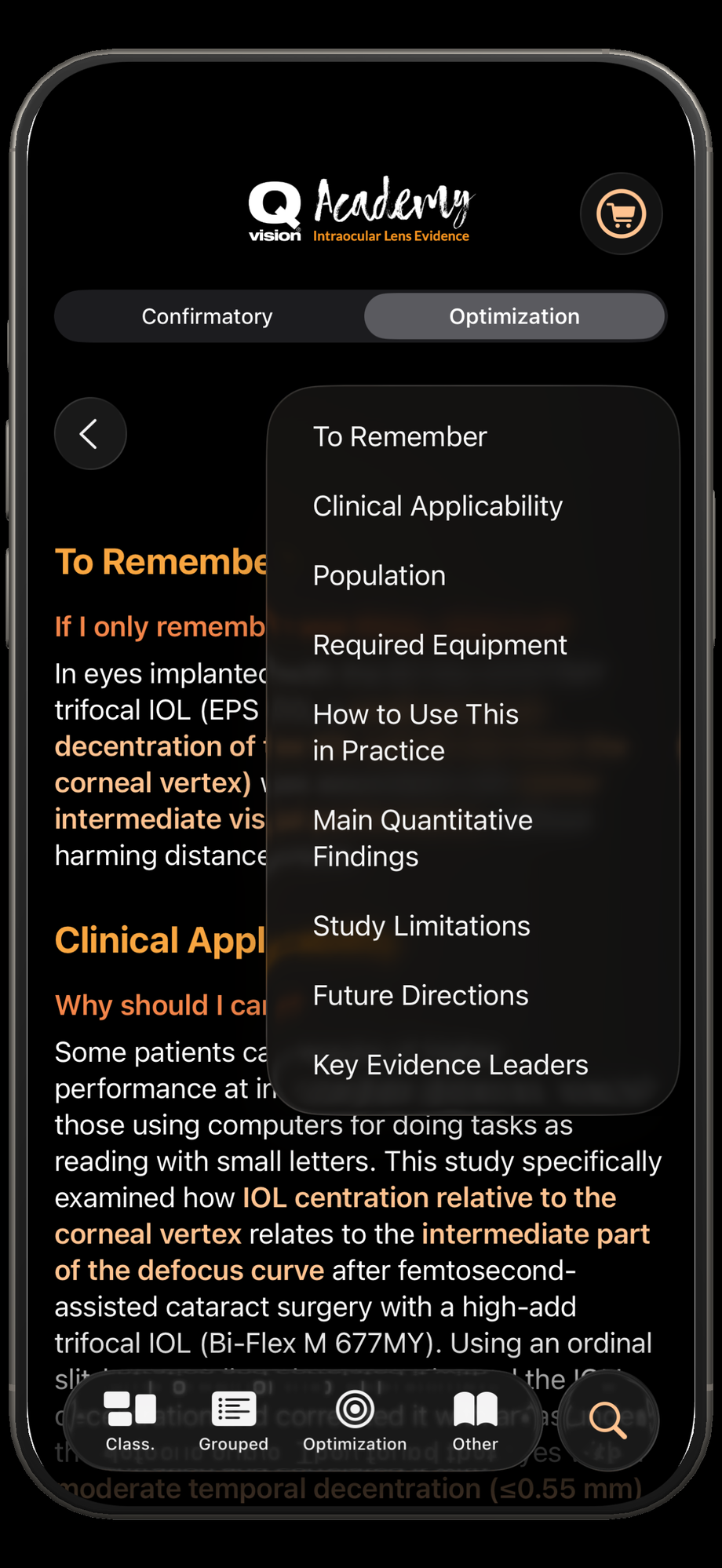
1.4.1. To Remember
If I only remember one thing, what is it?
This section distills the study into a single, clinically meaningful sentence. It highlights the most important practical takeaway, focusing on how the findings may influence patient selection, surgical planning, or postoperative expectations.
The goal is to allow clinicians to quickly grasp the core message of the paper without reading the full report.
1.4.2. Clinical Applicability
Why should I care?
This section explains the clinical problem addressed by the study, why it is relevant, and how the findings contribute to current practice. It contextualizes the research within real-world decision-making, such as managing patient dissatisfaction, understanding unexpected visual outcomes, or refining indications for specific IOL designs.
1.4.3 Population
Who does this apply to?
Here, the characteristics of the study population are clearly described, including age range, ocular condition, baseline visual status, and key inclusion or exclusion criteria. This allows clinicians to judge whether their own patients resemble those studied.
Special attention is given to factors that may limit generalizability, such as highly selected populations, post-refractive surgery eyes, or patients with specific biometric or optical characteristics.
1.4.4. Required Equipment
What do I need to apply this in practice?
This section outlines the devices, tests, or tools required to reproduce or apply the study findings in routine clinical care. This may include visual acuity charts, contrast sensitivity tests, aberrometers, pupillometry, questionnaires, or imaging systems.
When applicable, acceptable alternatives are mentioned, helping clinicians adapt the findings to different clinical settings.
1.4.5. How to Use This in Practice
What steps should I follow?
This section translates the study’s implications into clear, actionable clinical steps. These steps may include how to evaluate patients preoperatively, how to interpret specific measurements, or how to adjust surgical or refractive strategies based on the findings. Information is presented in short, ordered bullet points to facilitate rapid reading and implementation.
1.4.6. Main Quantitative Findings
What are the key numbers?
This section summarizes the most clinically relevant numerical results, such as thresholds, effect sizes, percentages, or comparative differences. Only results that directly influence interpretation or decision-making are included.
Rather than exhaustive statistics, the focus is on numbers that help clinicians understand how large an effect is and when it becomes clinically meaningful.
1.4.7. Study Limitations
How much can I trust this?
This section provides a balanced overview of the main limitations of the study, such as design constraints, sample size, follow-up duration, measurement variability, or potential sources of bias.
Understanding these limitations helps clinicians apply the findings appropriately, avoiding overinterpretation or misuse.
1.4.8 Future Directions
How firm are these recommendations?
Here, the report discusses what remains uncertain and what additional research is needed to strengthen or refine the conclusions. This may include the need for prospective studies, longer follow-up, broader populations, or standardized methodologies.
This section helps clinicians understand whether the findings represent an emerging concept or a well-established principle.
1.4.9 Key Evidence Leaders
Who is behind this work?
The final section identifies the main authors, senior investigators, or research groups responsible for the study, as well as relevant landmark publications when appropriate.
This provides transparency, context, and a reference point for clinicians who wish to explore the topic further.
Expert Comments
An Expert Comment is a short, clinician-facing note that helps the reader interpret a study’s findings appropriately. Its purpose is not to judge the authors or restate the results, but to highlight the key practical takeaways and the interpretive nuances that matter when applying the evidence to real-world decision making.
What an Expert Comment does
Connects results to clinical meaning: It explains what the findings likely mean for practice, patient selection, diagnostics, or treatment planning.
Flags important “watch-outs”: It draws attention to aspects that may influence interpretation, such as population characteristics, measurement methods, comparability across devices, thresholds, or generalizability.
Supports balanced interpretation: It clarifies what the study supports with higher confidence and where caution, context, or local validation is advisable.
What an Expert Comment is not
Not a critique or blame statement: Avoid phrasing such as “the authors failed to…” or “the authors did this wrong…”, which can be opinion-based and adversarial.
Not a re-summary of the paper: It should not simply repeat the abstract in different words.
Not personal preference: It should not argue for a method based only on preference, unless clearly tied to the study’s data and clinical context.
Tone and style
Constructive and neutral: Use language like “readers should note…”, “a point to consider is…”, “this may influence…”.
Clinically oriented: Focus on what the reader needs to know to avoid misapplication of results.
Specific, not vague: Point to concrete factors (population, device, constants, endpoints, follow-up, thresholds) rather than generic statements.
Typical structure (2–5 sentences)
One-line take-home interpretation of the main finding in practical terms.
One or two interpretive alerts that could change how the result is applied (e.g., interchangeability assumptions, systematic bias vs limits of agreement, subgroup relevance, workflow differences).
Optional: A practical implication (for example, “standardize measurements,” “validate locally,” “avoid mixing devices without calibration”).
Example “watch-out” phrases
“A key point for interpretation is…”
“Readers should be aware that…”
“This finding may depend on…”
“When comparing with other studies, consider…”
“This is most applicable to patients who…”
Eligibility for including an Expert Comment in an Optimization Report
To include an Expert Comment within an Optimization Report, the contributor should meet a minimum evidence-leadership threshold: coauthorship on at least 5 peer-reviewed studies related to IOLs. This criterion helps ensure the comment is grounded in sustained, field-specific research experience and aligns with the report’s aim of practice-oriented optimization rather than personal preference. The comments should be based on the complete Original Study and not based on the Optimization report, therefore Experts should have read first the Original Study.
You can request including your Expert Comment through the chat system shown at the bottom right side of the website.
