4.2. How to improve the IOLEvidence Score
This IOLEvidence Score recommendations applies to IOLEvidence version 26.2 and later; earlier versions compute the score using quality of reporting only and do not include the Risk of Bias component.
4.2.1. Structure of the Score
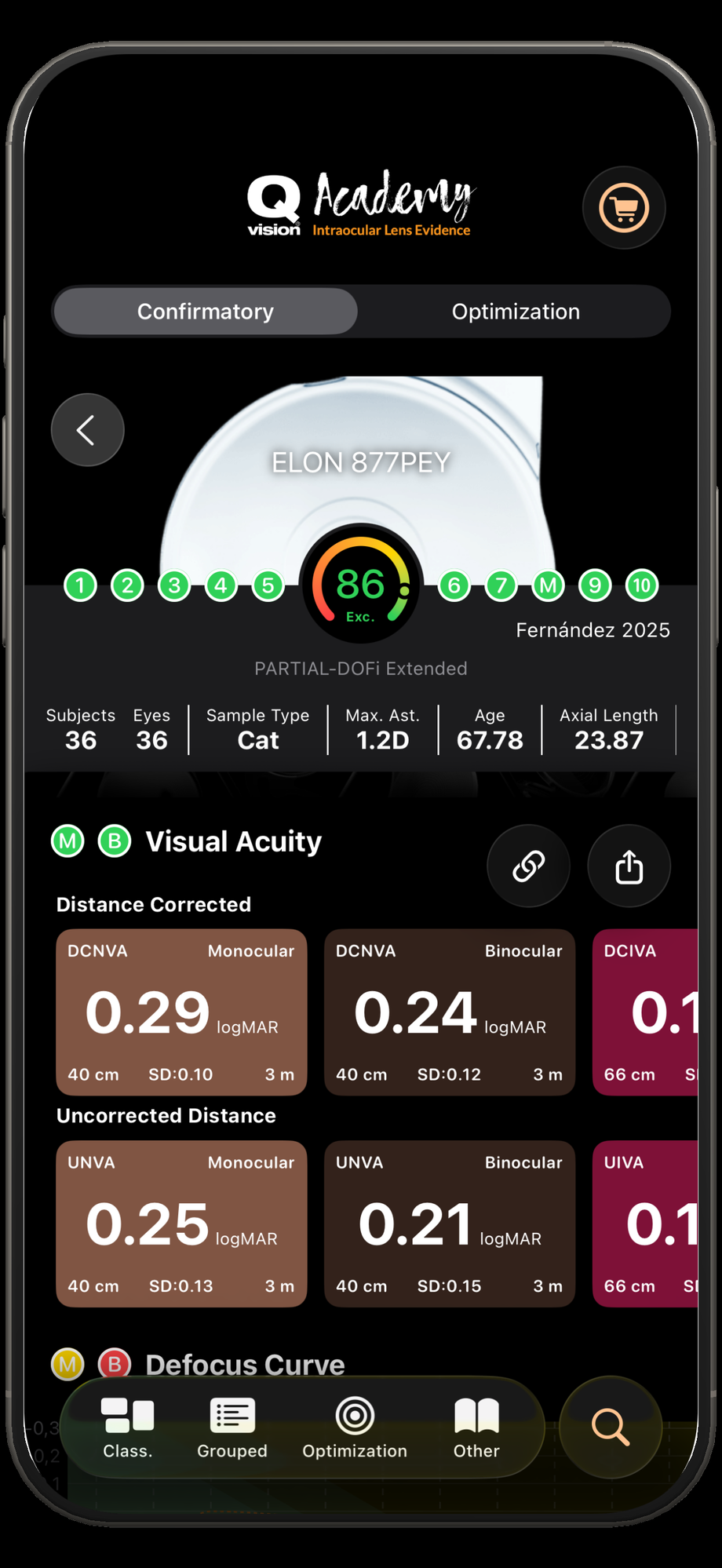
The Study Quality Score is a single value from 0 to 100, where:
Higher score indicates better quality of reporting and/or lower risk of bias
Lower score indicates poorer quality of reporting and/or higher risk of bias
The score is computed by combining two complementary components:
Reporting and Appraisal Component
This component evaluates whether essential methodological and reporting information is present and sufficiently detailed. It is based on 10 appraisal domains, each producing a normalized value (0–1). For each domain, results are classified as:
Yes → adequately reported
Unclear → partially reported
No → not reported
Some elements are weighted more heavily when they are critical for interpretation and evidence synthesis.
Risk of Bias Component
This component adjusts the score using study features associated with higher or lower risk of bias. It focuses on characteristics related to study design and conduct that can systematically influence results. In the final score, this component is aligned so that better design and lower bias risk increase the score, while higher bias risk decreases it.
 |  |
|---|
4.2.2. Appraisal Domains Explained in Detail (Reporting and Appraisal Component)
4.2.2.1. Inclusion Criteria
This domain evaluates whether the study clearly reports inclusion and exclusion criteria for the study. Special attention is given to factors that can strongly influence outcomes in IOL studies, including:
Presence or exclusion of ocular comorbidities
Preoperative corneal astigmatism and residual astigmatism
Planned postoperative refractive target or surgical plan
Reporting and handling of adverse events
Inclusion or exclusion of eyes with prior Nd:YAG capsulotomy
In the algorithm, these elements are independently weighted, meaning partial reporting results in an intermediate score.
Why it matters: Without clearly defined inclusion criteria, results cannot be contextualized or compared across studies.
4.2.2.2. Definition of the condition
This domain assesses whether the clinical condition under study is clearly defined and appropriate. In IOLEvidence, the condition is cataract surgery or refractive lens exchange for presbyopia correction.
The algorithm checks whether the study explicitly reports the condition (e.g. cataract diagnosis) in a way that is coherent with baseline visual status.
Why it matters: Ambiguity in the definition of the surgical indication limits interpretability of outcomes.
4.2.2.3. Identification of the condition
This domain evaluates whether valid methods are used to identify the condition for all participants. Specifically, it checks for reporting of:
Preoperative corrected distance visual acuity (CDVA)
Variability of CDVA (standard deviation)
Both elements are weighted, reflecting that reporting a mean alone is insufficient.
Why it matters: Baseline CDVA is essential to understand postoperative change and outcome interpretation.
4.2.2.4. Consecutive inclusion of participants
This domain evaluates whether participants were included consecutively over a defined period. The algorithm distinguishes between:
Explicit confirmation of consecutive inclusion
Unclear reporting
Evidence of selective inclusion
Why it matters: Non-consecutive inclusion may introduce selection bias and distort outcome distributions.
4.2.2.5. Complete inclusion of participants
This domain assesses whether all eligible participants were included and whether follow-up was complete. The algorithm rewards:
Explicit reporting of no recruitment loss or follow-up loss
Penalizes missing or unclear follow-up information
Why it matters: Loss to follow-up can systematically bias reported outcomes.
4.2.2.6. Demographic reporting
This domain evaluates the completeness of demographic and biometric reporting, with differential weighting based on clinical relevance. These demographic and biometric variables include:
Age and its variability
Photopic and mesopic pupil diameter
Axial length or IOL power
Sex distribution
Anterior chamber depth
Keratometry
Corneal astigmatism
Measurement device information
Why it matters: Demographic and biometric variables are key confounders in IOL performance and outcome variability.
4.2.2.7. Clinical and surgical information
This domain assesses reporting of surgical planning and execution details that may influence outcomes, including:
Planned refractive target and its variability
Formula and lens constant used
Number of surgeons
Surgical technique (phacoemulsification, incision type)
Capsulotomy size
Higher weight is assigned to elements directly influencing refractive accuracy.
Why it matters: Inadequate reporting of surgical parameters limits reproducibility and interpretation.
4.2.2.8. Outcome and follow-up reporting
This is one of the most heavily weighted and complex domains, and it is endpoint-specific. The algorithm adapts scoring logic depending on whether the outcome is:
Visual acuity
Contrast sensitivity
Defocus curve
Patient-reported outcomes
Measurement conditions (monocular vs binocular)
Follow-up duration
Use of standardized tests (e.g. ETDRS)
Luminance conditions
Reporting of mean values and variability
Control of memorization bias in defocus curves
Why it matters: Outcomes are only interpretable if measurement conditions and reporting standards are clearly defined.
4.2.2.9. Reporting of study site(s)
This domain assesses whether the clinical site or center(s) where the study was conducted are clearly reported.
Why it matters: Site information provides context on patient population, practice patterns, and external validity.
4.2.2.10. Statistical analysis
This domain evaluates whether the statistical analysis is appropriate and sufficiently reported, including:
Explicit statement of acceptable statistical methods
Reporting of sample size (eyes and subjects)
Inclusion of dispersion metrics (SD or CI)
The algorithm gives substantial weight to statistical adequacy.
Why it matters: Without proper statistical reporting, quantitative results cannot be reliably interpreted or synthesized.
4.2.3. Risk of Bias Component
In addition to reporting completeness, the score incorporates design and conduct signals that can influence risk of bias. This component typically accounts for:
Temporal design clarity (e.g., prospective vs retrospective vs unclear)
Standardization of outcome measurement (e.g., ETDRS use and controlled measurement conditions such as luminance)
Appropriateness and transparency of statistical methods
Sample size considerations (number of subjects and/or eyes)
Recruitment method quality (e.g., consecutive inclusion vs selective or unclear inclusion)
Endpoint reporting level (monocular and/or binocular outcomes when relevant)
Study design category (e.g., randomized vs case series)
End-point specific safeguards (e.g., measures addressing memorization effects when applicable for defocus curves)
These elements are incorporated so that studies with stronger design features and lower bias susceptibility receive a higher final score, even when reporting completeness is similar.
4.2.4.Recommendations for Authors
We recommend authors to follow established checklists and reporting standards for measuring and presenting outcomes in studies involving intraocular lenses. Adhering to these standards ensures transparency, completeness, and comparability of reported results, facilitating correct interpretation and evidence synthesis.
In particular, authors are encouraged to follow the methodological and reporting recommendations described in the following publications:
Sentence to include in the manuscript
“This study was designed, conducted, and reported in accordance with published recommendations and standards for collecting and reporting outcomes in intraocular lens–based refractive surgery.1,2
1. Fernández, J., Rocha-De-Lossada, C. & Rodríguez-Vallejo, M. Recommendations for Writing Clinical Research Manuscripts: From Monofocal to Multifocal Intraocular Lenses. Int. J. Environ. Res. Public Health 19, 17036 (2022).
2. Fernández, J. et al. Standard for collecting and reporting outcomes of IOL–based refractive surgery: update for enhanced monofocal, EDOF, and multifocal IOLs. J Cataract Refract Surg 48, 1235–1241 (2022).
